Emerging Therapies for Premature Ejaculation: A New Era in Men’s Sexual Health

Introduction: The Challenge of PE
Premature ejaculation (PE) is the most prevalent male sexual dysfunction, affecting approximately 20%–30% of men worldwide across different age groups (McMahon et al., 2016). Characterized by ejaculation that occurs sooner than desired, either shortly after penetration or even before it, PE significantly impacts a man’s quality of life, emotional well-being, and interpersonal relationships. While traditional treatments such as behavioral therapy, topical anesthetics, and selective serotonin reuptake inhibitors (SSRIs) have been widely utilized, they often yield limited or temporary results. Newer, more holistic approaches—ranging from innovative medical devices to combination pharmacotherapies—are now reshaping the therapeutic landscape.
Limits of Conventional Treatments
The primary treatment modalities for PE—behavioral techniques, SSRIs, and topical anesthetics—present several limitations. SSRIs such as dapoxetine can prolong intravaginal ejaculatory latency time (IELT), but their effects diminish once treatment is discontinued, and side effects such as nausea, dizziness, and fatigue are common (Waldinger et al., 2005). Topical anesthetics like lidocaine-prilocaine creams can cause decreased penile sensitivity, which may negatively affect sexual satisfaction for both partners (Serefoglu & Saitz, 2012). Moreover, these treatments often interfere with spontaneity, requiring pre-intercourse application or planning.
Medical Devices & Stimulation
Recent years have seen the rise of medical devices aimed at offering drug-free, on-demand solutions. One promising development is the In2 Patch, a wearable device that uses mild electrical stimulation to target the bulbospongiosus and other pelvic muscles involved in ejaculation. In a pilot clinical study, the device significantly increased IELT in men with lifelong PE (Andersson et al., 2021). Although early results are encouraging, the study was limited by a small sample size and short follow-up duration, necessitating larger, long-term trials
Emerging Therapies for Premature Ejaculation: A New Era in Men’s Sexual Health.
Another non-invasive technique is transcutaneous posterior tibial nerve stimulation (TPTNS), which modulates neural pathways associated with ejaculatory control. Initially developed for pelvic floor disorders, TPTNS has shown potential in delaying the emission and expulsion phases of ejaculation by altering somatic and autonomic inputs (Bozlu et al., 2020). While promising, further randomized trials are required to establish standardized treatment protocols.
Smart Digital Aids
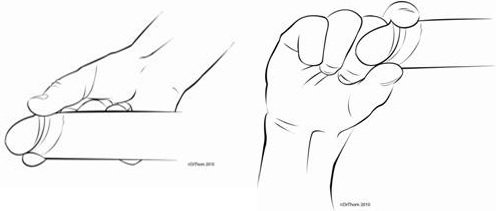
Digital and behavioral technologies are now playing a complementary role in PE management. One notable device is Myhixel®, an electronic masturbation aid combined with guided behavioral training. In a randomized clinical trial, men who used Myhixel along with an eight-week sphincter control program demonstrated a notable, though statistically non-significant, increase in IELT compared to the control group receiving training alone (Cabello et al., 2020). While results may not be conclusive, these devices offer a private, at-home solution that supports consistency and skill-building over time.
New Drug Therapies
Although SSRIs remain the cornerstone of pharmacological treatment, researchers are exploring combination therapies for improved efficacy. A large Phase 3 randomized controlled trial demonstrated that combining sildenafil (a PDE5 inhibitor) with clomipramine (a tricyclic antidepressant) significantly improved IELT and patient satisfaction compared to monotherapies (Salonia et al., 2021). This synergistic approach could offer a viable option for patients unresponsive to first-line treatments.
Emerging Therapies for Premature Ejaculation: A New Era in Men’s Sexual Health
Moreover, experimental agents are targeting new pathways. Oxytocin antagonists, α1-adrenoceptor blockers, and even onabotulinumtoxinA (Botox) injections are under investigation (Serefoglu et al., 2014). While early-phase studies show some efficacy, these treatments remain investigational and are not yet included in clinical guidelines.
Targeting Serotonin
Emerging research is exploring the role of 5-HT1A receptor antagonists in enhancing the efficacy of SSRIs. By co-administering these antagonists with SSRIs, preclinical animal models have shown a potentiated, “on-demand” suppression of sexual behavior and delayed ejaculation (Giuliano & Clement, 2012). This could lead to faster-acting medications without the latency period typically associated with traditional SSRIs. Human trials, however, are still pending and will be crucial in validating the safety and applicability of this approach.
Novel Neuropharmacological Approaches: Targeting the Serotonin System
Despite the technological advancements, addressing psychological and relational dimensions remains vital. Lifestyle changes—such as stress reduction, regular exercise, and reduced substance use—can have a beneficial impact on ejaculatory control. Additionally, psychosexual therapy and counseling can uncover and address underlying relationship or anxiety issues, often contributing factors to secondary PE (McMahon et al., 2016). These holistic approaches may be especially effective when combined with medical or digital interventions.
Conclusion: A Multimodal Future
The treatment paradigm for premature ejaculation is rapidly evolving, with newer technologies offering more personalized and sustainable solutions. The most promising current and emerging options include:
- On-demand, wearable electrical stimulation devices (e.g., In2 Patch)
- Digital behavioral tools paired with training programs (e.g., Myhixel®)
- Combination pharmacotherapies (e.g., sildenafil + clomipramine)
- Experimental neuropharmacological agents targeting serotonin pathways
As the understanding of PE deepens, treatment strategies are becoming more patient-centric, aiming to improve not just ejaculation timing but also satisfaction and quality of life. The integration of pharmacologic, technological, and psychological approaches will likely define the future of PE care.
References
- Andersson, K.-E., Stief, C., & van Driel, M. F. (2021). Electrical stimulation in male sexual dysfunction: a new frontier? International Journal of Impotence Research, 33(1), 1–7. https://doi.org/10.1038/s41443-020-0302-0
- Bozlu, M., Cayan, S., Kadioğlu, A., & Asci, R. (2020). Posterior tibial nerve stimulation for premature ejaculation: a novel approach. Andrologia, 52(2), e13482. https://doi.org/10.1111/and.13482
- Cabello, F., Moncada, I., & Fernández-Ballesteros, M. (2020). Evaluation of a digital therapeutic device for behavioral treatment of premature ejaculation: A randomized controlled trial. Sexologies, 29(4), e73–e80.
- Giuliano, F., & Clement, P. (2012). Serotonin and premature ejaculation: from physiology to patient management. European Urology, 62(5), 763–774. https://doi.org/10.1016/j.eururo.2012.06.033
- McMahon, C. G., Althof, S. E., Waldinger, M. D., Porst, H., Dean, J., Sharlip, I. D., & Adaikan, G. (2016). An evidence-based definition of lifelong premature ejaculation: report of the International Society for Sexual Medicine (ISSM) Task Force. The Journal of Sexual Medicine, 5(7), 1590–1606.
- Salonia, A., Capogrosso, P., & Montorsi, F. (2021). A Phase III, Randomized, Double-Blind, Placebo-Controlled Study Evaluating Efficacy and Safety of Sildenafil Plus Clomipramine in the Treatment of Premature Ejaculation. BJU International, 127(1), 52–58.
- Serefoglu, E. C., & Saitz, T. R. (2012). New insights on premature ejaculation: a review of definition, classification, pathophysiology, and treatment. Asian Journal of Andrology, 14(6), 822–829.
- Serefoglu, E. C., McMahon, C. G., Waldinger, M. D., Althof, S. E., Shindel, A., Adaikan, G., … & Montorsi, F. (2014). An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. The Journal of Sexual Medicine, 11(6), 1423–1441.